We’re pleased to present the table of contents and abstracts from the latest issue of IJFAB: International Journal of Feminist Approaches to Bioethics. For the full issue, see University of Toronto Journals.
Dirk Lafaut & Gily Coene, “Autonomy Without Borders? Understanding the Impact of Undocumented Residence Status on Healthcare Relationships in Belgium”
https://doi.org/10.3138/ijfab-2023-03-20
“Access to public healthcare services for Belgium’s undocumented migrants is regulated through a parallel, administrative procedure within the legal framework of Urgent Medical Aid. This imposes several constraints on their access to healthcare services. Drawing on empirical-ethical methodologies, we show how this procedure impacts on the relationship between patients with undocumented status and healthcare workers. We use the concept of relational autonomy to show how the imposed legal constraints reduce the formal treatment options available to healthcare workers, but simultaneously lead to informal care practices, and how the latter increase the discretionary power of the healthcare workers. We argue that in this context, provision becomes unpredictable and arbitrary, with undocumented migrants tending to value strong personal relations with one particular, trusted healthcare worker. Although this leads to increased dependence, it also increases patients’ options and autonomy by providing access to wider professional networks attached to that healthcare worker.”
Keywords: agency, Belgium, bioethics, healthcare access, relational autonomy, undocumented migrant
Vicki Toscano, “The Responsibility Objection to Thomson Re-imagined: What If Men Were Held to a Parallel Standard?”
https://doi.org/10.3138/ijfab-2022-0011
“This article focuses on a resonant debate initiated by the publication of Judith Jarvis Thomson’s groundbreaking article “On Defense of Abortion” in 1971. It is my contention that philosophers who argued against Thomson based on what has come to be called the “Responsibility Objection” did not fully examine the gender assumptions embedded in their logic. Rather than attempt to prove the flaw in the Responsibility Objection directly, I demonstrate it by applying the same logic used to discuss women’s responsibilities to men to prove that it also supports forcing men to get a vasectomy. What I show is that the Responsibility Objection, when no longer clothed in a set of gendered assumptions, is not logically convincing. Further, given that the Responsibility Objection supports the logic the U.S. Supreme Court recently relied on in Dobbs vs. Jackson Women’s Health in overruling Roe vs. Wade, the examination of the flaws in this logic is timely and important.”
Keywords: abortion, Judith Jarvis Thomson, responsibility objection, Dobbs vs. Jackson Women’s Health, vasectomy
Wendy A. Rogers & Jacqueline Dalziell, “What Feminist Bioethics Can Bring to Synthetic Biology”
https://doi.org/10.3138/ijfab-2023-0004
“Synthetic biology (synbio) involves designing and creating new living systems to serve human ends, using techniques including molecular biology, genomics, and engineering. Existing bioethical analyses of synbio focus largely on balancing benefits against harms, the dual-use dilemma, and metaphysical questions about creating and commercializing synthetic organisms. We argue that these approaches fail to consider key feminist concerns. We ground our normative claims in two case studies, focusing on the public good, who holds and wields power, and synbio research projects’ particularity and context. Attention to feminist concerns is essential for synbio to realize its potential in ethically justifiable ways.”
Keywords: ethics of synthetic biology, feminist bioethics, case studies, empirical bioethics research, research for the public good
Johnny Brennan, Molly Kelleher, Rossio Motta-Ochoa, Stefanie Blain-Moraes & Laura Specker Sullivan, “Situated Personhood: Insights from Caregivers of Minimally Communicative Individuals”
https://doi.org/10.3138/ijfab-2022-0016
“For caregivers of minimally communicative individuals, providing support in the absence of clearly meaningful responses is ethically fraught. We conducted a secondary analysis of qualitative data from caregivers of individuals who are minimally communicative, including persons with advanced dementia and individuals in disorders of consciousness. Our analysis led to two central claims: (1) Personhood is a threshold concept that is situated, relational, and dynamic and (2) in circumstances in which personhood is difficult to judge, caregivers can “fill the gap” to reach the threshold through a repertoire of strategies. Because personhood is in part an attribution from others, a situational loss of personhood does not preclude restoration, nor does it eliminate moral status.”
Keywords: personhood, caregiving, moral status, disability
Yingyi Luo, Denise Cuthbert & Shelley Marshall, “The Representation of Cross-Border Surrogacy in Australian Surrogacy Events”
https://doi.org/10.3138/ijfab-2022-0030
“As a method of family formation, cross-border surrogacy is controversial and beset by risks of exploitation. This article extends the literature on surrogacy by examining the way Australian surrogacy promotion and information events represent cross-border surrogacy. It examines the emerging phenomenon of surrogacy events held by a not-for-profit surrogacy organization to promote cross-border surrogacy in Australia—a country that prohibits commercial surrogacy. The article draws on observations from a series of surrogacy events in Australia and online during the 2019–21 time period. It examines the presentations given at these events by surrogacy facilitators, surrogate mothers, and intended parents. We observed four themes: (1) Intended parents are positioned as consumers, (2) the benefits of cross-border commercial surrogacy are highlighted relative to other methods of family formation, (3) the positive side of cross-border surrogacy is accentuated, and (4) reproductive rights are emphasized. These representations run counter to feminist framings of cross-border surrogacy as exploitative and risky. This paper understands that the framing of surrogacy that occurs at these promotion events to be neoliberal in nature. The conceptualization helps explain their consumerist peppiness and commodifying subjectivity.”
Keywords: feminist, surrogacy events, cross-border surrogacy, Australia, not-for-profit organization
Chantal Bayard & Phyllis L.F. Rippey, “Cornering the Market on Maternal Affect: A Discourse Analysis of a Social Media Marketing Campaign for Infant Formula”
https://doi.org/10.3138/ijfab-2022-0015
“Breastfeeding advocates and global health agencies have been sounding alarms about the dangers of digital marketing practices of the formula-feeding industry. This study comprised a feminist discourse analysis of materials produced (blog, social media posts, comments) in a paid partnership between baby formula brand Enfamil and an influencer, Marilou Bourdon from Trois fois par jour. Our analysis reveals a sophisticated marketing campaign that co-opts feminist critiques of breastfeeding promotion discourse while carefully avoiding explicitly violating the International Code of Marketing of Breast-milk Substitutes. Underlying this campaign is a rhetoric reliant on pathos to assuage maternal guilt and shame for feeding formula.”
Keywords: breastfeeding, infant formula, emotion, marketing, social media
Olivia Schuman, “Should Bionormativity Be a Concern in Gamete Donation?”
https://doi.org/10.3138/ijfab-2023-0009
“An important argument against removing donor anonymity is that such state-mandated policies might validate bionormative attitudes about the importance of genetic relatedness in families. Bionormative attitudes can be unjustly disparaging and harmful to a wide range of families including donor-conceived, adopted, and single-parent families. However, studies show that the majority of donor-conceived individuals want donor anonymity removed. This paper explores the question of how to weigh these desires for knowing the donor—which may be grounded in biased and bionormative assumptions—against the competing concern that removing donor anonymity perpetuates attitudes that may be harmful.”
Keywords: gamete donation, reproductive ethics, family ethics, genetic information
Natalie Dorfman & Joel Michael Reynolds, Commentary: “The New Hysteria: Borderline Personality Disorder and Epistemic Injustice”
https://doi.org/10.3138/ijfab-2023-0008
“The diagnostic category of borderline personality disorder (BPD) has come under increasing criticism in recent years. In this paper, we analyze the role and impact of epistemic injustice, specifically testimonial injustice, in relation to the diagnosis of BPD. We first offer a critical sociological and historical account, detailing and expanding a range of arguments that BPD is problematic nosologically. We then turn to explore the epistemic injustices that can result from a BPD diagnosis, showing how they can lead to experiences of testimonial injustice which impede patient engagement in meaning-making activities, thereby undermining standard therapeutic goals. We conclude by showing how our arguments bolster ongoing efforts to replace the diagnostic category of BPD with alternatives such as complex post-traumatic stress disorder.”
Keywords: epistemic injustice, sexism, borderline personality disorder, diagnosis, post-traumatic stress disorder
Moira Kyweluk & Autumn Fiester, Commentary: “The Ethical Mandate of Fertility Preservation Coverage for Transgender and Gender Diverse Individuals”
https://doi.org/10.3138/ijfab-2022-0009
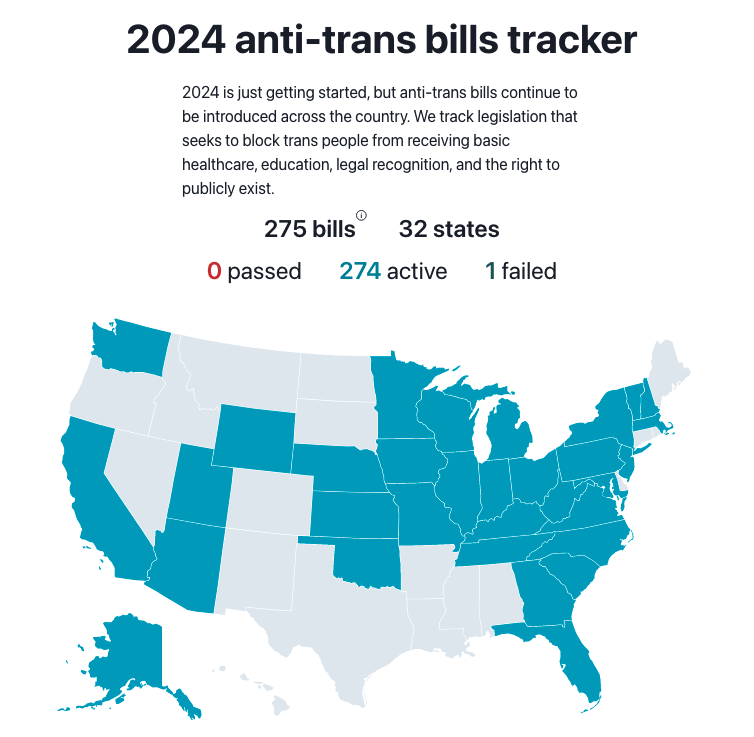
“For individuals pursuing medically assisted gender transition, gender-affirming surgical treatments, such as oophorectomy (removal of the ovaries) and orchiectomy (removal of the testicles), cause sterility, and gender-affirming hormone treatment with medications (i.e., testosterone and estrogen) may negatively impact infertility. The major United States (US) medical associations already endorse fertility preservation (FP) through cryopreservation (i.e., “freezing” egg and sperm) for transgender individuals. Despite these endorsements from the relevant medical societies, medical insurance coverage for FP remains very limited in the US. Given the high out-of-pocket costs for FP services, fertility preservation remains financially out of reach for many transgender individuals who may desire it. We present an ethical justification for universal FP coverage for all transgender and gender diverse (TGD) individuals who request this option during medically assisted gender transition. First, we argue that gender-affirming medical care is analogous to other medical interventions and treatment regimens that compromise fertility, such as cancer care, and that both types of interventions need to be afforded the same medical benefits and assistance in pursuing fertility goals. Second, we argue that the lack of FP for transgender individuals contributes to the ongoing and profound transphobia and anti-trans bias that has been exacerbated in the past several years across the healthcare landscape in the United States. We argue that the provision of FP coverage for transgender individuals is necessary for clinicians and third-party payers to state their unequivocal support for TGD patients and their healthcare needs.”
Keywords: clinical ethics, fertility coverage, queer bioethics, reproductive justice, trans health
Michael DeProost, Commentary: “Male Fertility-Related mHealth: Does it Create New Vulnerabilities?”
https://doi.org/10.3138/ijfab-2022-0028
“Male fertility–related mHealth (MFmHealth), including smartphone applications that allow men to test their fertility at home, is getting some attention now and then. In this commentary, I argue that MFmHealth technology has the potential to undermine established norms around male reproduction but cannot be examined using traditional individualist frameworks in bioethics. Instead, theoretical literature on the concept of vulnerability in feminist bioethics allow a theoretical alliance with critical studies of men and masculinities. Proposed benefits like empowerment, shared responsibility, and democratization may justify disruptive innovation but may also obscure more fundamental ethical concerns about vulnerability and social justice.”
Keywords: male fertility–related mHealth, masculinity, paternal effects, social justice, vulnerability
Rebecca Simmons, review of Abortion to Abolition: Reproductive Health and Justice in Canada by Martha Paynter
https://doi.org/10.3138/ijfab-2022-0029