
Lauren Freeman 
Heather Stewart
This guest blog comes to IJFAB from Lauren Freeman and Heather Stewart, and conveys the core of the argument they render in a recent issue of the Kennedy Institute of Ethics Journal. Freeman is Associate Professor of Philosophy at the University of Louisville and a core member of the MA in Bioethics and Medical Humanities. Stewart is a PhD student at the University of Western Ontario, whose work in medical ethics focuses on delivery of care to members of queer and trans communities. Freeman and Stewart are co-authoring a book called Microaggressions in Medicine.
‘Microaggression’ is a term that gets thrown around a lot these days, especially on college campuses. The term refers to routine and seemingly insignificant comments or gestures, sometimes intentional, but mostly unintentional, that convey negative messages to targets, who are members of one or more marginalized group.

Many people, especially those on the receiving end, know that microaggressions are real. In fact, their everyday experiences are often shaped, colored, and constrained by the negative content of microaggressions, even though microaggressive acts are often committed by well-intentioned individuals, sometimes even by their friends, family members, or colleagues.
But there’s also a large number of people who doubt the very existence or seriousness of microaggressions. These critics claim that what we have on our hands is an overly sensitive generation of snowflakes who just need to calm down, grow a spine, and stop taking everything so personally.
Our recently published article in The Kennedy Institute of Ethics Journal (KIEJ), “Microaggressions in Clinical Medicine,” proposes a new way of understanding microaggressions, one that aims to respond to critics who doubt the reality of the phenomenon. Our goal is to convince critics both that microaggressions are real and also that they can cause serious and enduring harm to those on the receiving end. The context of our discussion is medicine, but we think that microaggressions occur most everywhere.
One problem with the way that microaggressions tend to be discussed is that they almost always begin from and prioritize the perspective of the one enacting them, namely, the more dominant person in the given relation of power. The standard taxonomy for categorizing microaggressions, developed by Derald W. Sue (2007, 2010), is divided into microinsults, microinvalidations, and microassaults (a term that we think is an oxymoron since no assault can be ‘micro’). Notice that on this sort of view, in addition to starting from the perspective of the one who holds a position of (relative) power and privilege, microaggressions are defined on the basis of the act committed: an insult, invalidation, or assault, respectively.
We believe that conceptualizing microaggressions from the perspective of the microaggressor, (an act- or agent-based model), gets off on the wrong foot. Most notably, it takes the central focus away from the victim – presumably precisely where the focus of an account of microaggressions should be.
A consequence of the dominant model of microaggressions that centers on the perspective of the microaggressor and pushes targets or victims to the side, is that it becomes easier for critics of microaggressions to blame the victims, to deny their experiences, or to be critical of (the severity of) their responses to microaggressions. As a result, and again, insofar as the perspective of the microaggressor is prioritized, it becomes more difficult to zero in on precisely what targets of microaggressions are experiencing from their own perspectives and how and why microaggressions can cause such harm. Foregrounding the perspective of microaggressors makes it harder to empathize with targets of microaggressions, and easier to assume that they could or should just “toughen up” or grow “thicker skin.”
It’s worth noting (and not at all surprising) that the most vocal criticisms of microaggression research and activism have come from economically privileged, cis-het white men, most of whom, given their dominant social position, have never personally experienced systemic oppression or marginalization of any kind.
In contrast to the way microaggressions have been commonly understood for roughly the past decade, we offer a novel account of the phenomenon that starts from the perspective of victims and the various harms they experience. In so doing, we aim to put victims and their experiences at center stage. Doing so, we believe, makes it easier to see that harm is experienced as a result of being on the receiving end of microaggressions. It also makes it easier to categorize the distinct kinds of harm experienced. In our elaboration of this position, it becomes clear that these harms are both serious and enduring.
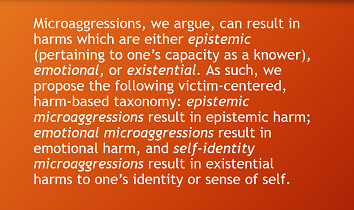
“Microaggressions in Clinical Medicine” sets out our alternative taxonomy for classifying microaggressions on the basis of their harmful effects – one that gets away from the dominant action- or agent-based model. Microaggressions, we argue, can result in harms which are either epistemic (pertaining to one’s capacity as a knower), emotional, or existential. As such, we propose the following victim-centered, harm-based taxonomy: epistemic microaggressions result in epistemic harm; emotional microaggressions result in emotional harm, and self-identity microaggressions result in existential harms to one’s identity or sense of self. Importantly, each type of microaggression can occur on the basis of stereotypes or biases pertaining to sex, race, body size, sexual orientation, gender identity, dis/ability, accent, and so on, or a combination thereof.
Centering our argument around a diverse set of testimonies from members of various marginalized groups, our paper develops an analysis of these three types of microaggressions and their resulting harms, specifically as they impact patients in medical environments. We argue that over time, the accumulation of microaggressions in medical contexts can have detrimental effects to physician-patient relationships: that is, repeated microaggressions can result in diminished trust, and, as a consequence, can undermine the kind and quality of care that patients receive.
In some cases, as we demonstrate, repeatedly being on the receiving end of microaggressions can even cause people to forego medical care entirely. This is particularly the case for women, African Americans, and trans folks who endure frequent microaggressions of all types in medical settings. It goes without saying, then, that we find it crucial for healthcare providers to have microaggressions on their radar, and, moreover, to do the work of understanding the various harms that can result from microaggressions and to actively try to stop committing them (as difficult as that may be).
In order to get a sense of how our victim-centered, harm-based account of microaggressions works, as well as the serious, long-term consequences of microaggressions in medical contexts, consider an example that we develop at length in our paper. The case involves a transgender woman, Xeph Kalma, who struggles with depression and suicidal ideation, and who brought herself to the emergency room in the midst of a suicidal episode.
Upon her arrival, Kalma made sure to tell the medical staff on several occasions to use her affirmed pronouns and name. Despite her efforts, she was repeatedly misgendered and deadnamed (that is, referred to using her birth name, which she no longer uses or identifies with). In her already difficult mental state, Kalma refers to the experiences of being casually and repeatedly misgendered and deadnamed by those responsible for her care as like “being hit with a hammer.”
This disorienting feeling that Kalma experienced is the result of having her medical team fail to recognize and respect core aspects of her identity. In her already suicidal state, those responsible for her care used pronouns and a name that reminded Kalma of very difficult times in her life – indeed, of a past life with which she no longer wants to identify. She states that this made her feel “worse than when [she] had arrived at the hospital.” As a result of having her identity repeatedly dismissed and undermined, she walked out of the hospital, with no intention of ever returning:
The way I was treated in the ER—the misgendering, deadnaming, ignorance, and the lack of discretion I experienced—is incredibly dangerous. When I say it was ‘my last visit,’ I mean it. I will not voluntarily return to an ER the next time I’m feeling suicidal. Anything would be a better option than experiencing that level of embarrassment and shame again. Embarrassment and shame, from those who were meant to take care of me.
Kalma’s testimony highlights the severity of patients’ experiences of and responses to one type of microaggressions in medical contexts. Microaggressions can be a matter of life and death.
What makes our account—one that begins with the harms to victims instead of being guided by the acts committed by microaggressors –conceptually stronger than the dominant action-based account, is that it’s better able to determine the precise nature of harm suffered by victims. As a result, it’s less likely for others to doubt or deny that any serious harm has occurred, or to assume that victims are making it up or that it’s all in their heads. Here’s why.
If we stick to Sue’s action-based taxonomy of microaggressions, it’s difficult to pinpoint the precise nature of the harm suffered by Kalma. On Sue’s account, deadnaming might count as a microinvalidation insofar as the victim’s personhood is invalidated by failing to recognize who she is; or possibly, it could count as a microassault, defined as an explicit “derogation characterized primarily by a verbal or nonverbal attack meant to hurt the intended victim through name-calling, avoidant behavior, or purposeful discriminatory actions” (Sue et al. 2010, 274).
In either case, to focus on what type of act the health care providers engaged in misses the morally salient point.
To be deadnamed and misgendered was profoundly harmful to Kalma’s general well-being, yet neither of Sue’s categories of microaggressions manages to capture the precise and enduring harm to Kalma that a self-identity microaggression and the resulting existential harm does. This is because on Sue’s account, both types of microaggressions collapse all types of harm under one general category. Whether Sue’s account would call what Kalma experienced a microinvalidation or microassault, all that it really tells us about her experience is that she was microaggressed in one of these ways. The account remains neutral on whether, and in what exact way, Kalma was harmed.
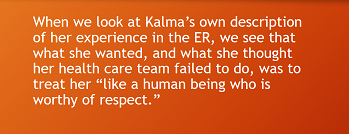
When we look at Kalma’s own description of her experience in the ER, we see that what she wanted, and what she thought her health care team failed to do, was to treat her “like a human being who is worthy of respect.” Using the language of self-identity microaggression and the resulting existential harm highlights that what occurred to Kalma had implications for her very identity and sense of self in a serious and lasting way.
An account that labels microaggressions on the basis of their harms is better able to capture what’s morally wrong in the case—a conclusion that isn’t as easily or readily reached when her experience is described using Sue’s more general language of microassault or microinvalidation, which speaks generally of “harm” as a singular category.
We take this foregrounding of the experiences of victims of microaggressions to be the central insight and strength of our account.
The KIEJ paper is part of a larger project we are undertaking, a book manuscript called Microaggressions in Medicine, whose aim is to overhaul the dominant conception of microaggressions and to provide an actionable account of microaggressions that can be operationalized to study the harms of microaggressions empirically. Ideally, our account can also be used to develop microaggression awareness trainings that center the perspectives and interests of those who are most likely to be harmed by pervasive microaggressions.
In sum, we hope that our work will serve both as a rebuttal to those who doubt or deny the reality and importance of microaggressions, in addition to laying the groundwork for a novel victim-centered, harm-based approach. We believe that such a shift to understanding and conceptualizing microaggressions from the perspective of victims will become a rich field of theorizing and advocacy, aimed at offsetting the many and serious harms of microaggressions that our work aims to illuminate.

